MHH research team develops new molecular tool to investigate the influence of telomerase on the development of heart muscle cells
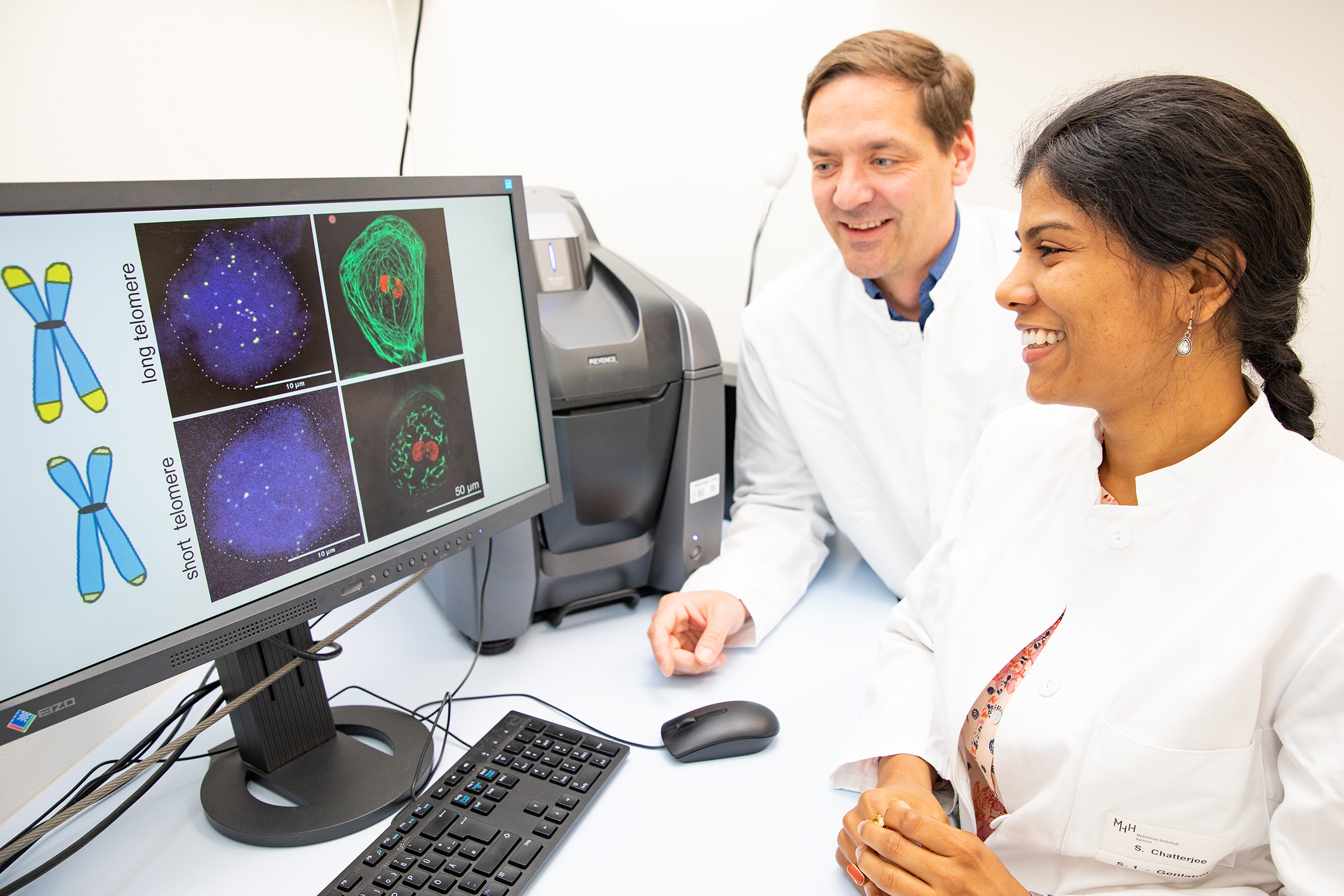
Professor Dr Christian Bär and Dr Shambhabi Chatterjee have developed a new tool to investigate the influence of the protective caps for our genetic material on heart health. Copyright: Karin Kaiser / MHH
As we age, our appearance changes, our hair turns grey and wrinkles appear. And we become more susceptible to disease. One reason for this is that our telomeres shorten. These are protective caps at the ends of the chromosomes, the carriers of our genetic material. Each time a cell divides, the telomeres become shorter until they reach a critical length and the genes they protect could be damaged. Then the cell stops dividing and the tissue ages. The length of the telomeres is therefore considered a marker for a person's biological age. Their shortening increases the risk of age-related diseases such as Alzheimer's or cancer as well as cardiovascular diseases.
In heart muscle cells, known as cardiomyocytes, telomere length is strongly linked to the performance of the heart. People with short telomeres in the heart muscle cells, for example, are more prone to heart failure. However, it is unclear whether short telomeres are the cause or the result of the disease. Researchers led by Professor Dr Christian Bär, molecular biologist at the Institute for Molecular and Translational Therapy Strategies at Hannover Medical School (MHH), want to solve this "chicken and egg problem". They have now made significant progress in this endeavour. They have developed a new molecular tool with which they can produce stem cells of different, precisely defined telomere lengths and then compare how fit the resulting heart muscle cells are. The results have been published in the journal "Cellular and Molecular Life Sciences".
Control element for telomere lengths
"In this study, we used human induced pluripotent stem cells, i.e. body cells that have been reprogrammed back to their original state, so to speak," explains Professor Bär. The researchers edited these "rejuvenated" hiPS cells, which can now develop into any human tissue again, using CRISPR gene scissors. However, they did not remove DNA from the hiPS cells, but inserted a control element that can specifically switch off the reading of a certain gene. The molecular tool regulates the production of telomerase, an enzyme that adds new DNA to the end of the telomere and thus lengthens it. As a result, the cell retains its ability to divide and does not age. In adults, telomerase is normally switched off and is only active in a few niches, for example in the haematopoietic stem cells in the bone marrow. With the help of the modified gene scissors, the researchers were able to generate so-called human CRISPR interference stem cells (CRISPR ihiPSC) with precisely defined telomere shortening, which in turn developed into heart muscle cells with correspondingly shorter or longer telomeres.
Telomerase can protect the heart
"Using these CRISPR ihiPSC-derived cardiomyocytes, we were able to investigate the effects of telomere length on the development of heart muscle cells and their response to stress stimuli," emphasises Professor Bär, who has been researching the protective caps of our DNA for more than ten years and heads the working group "The non-coding genome in cardiac ageing and regeneration". "We found that fully functional heart muscle cells only developed from ihiPSCs with long telomeres," says Dr Shambhabi Chatterjee, scientist in the working group and first author of the study. "Poor cardiomyocyte function and increased sensitivity to stress were therefore directly related to the extent of telomere shortening."
In previous work, Professor Bär and his colleague Dr Chatterjee have already discovered that reactivating telomerase can help against age-related diseases and protect the heart - at least in cell culture and in animal models. "We investigated the systemic reactivation of telomerase by loading so-called gene taxis with the telomerase gene and introducing them into mouse cells," explains the scientist. "This also significantly extended the lifespan of the animals in the mouse model, even in adult and aged mice, and had a protective effect on the heart even after a heart attack."
More reliable evaluation of cardiac drugs
The novel tool developed in this study for altering telomere length offers the possibility of reproducing related diseases such as heart failure in cell culture and examining them in a standardised way. "Previously, this required tissue samples from the heart, but these can differ greatly from person to person in terms of telomere length and are therefore only comparable to a limited extent," says Professor Bär. Another advantage of the test platform is that it can be used to produce genetically identical CRISPR ihiPSC-derived cardiomyocytes with long and short telomeres. These could, for example, be used as controls in the systematic testing of cardiac drugs and thus contribute to a more reliable evaluation of the drugs. He is also convinced that therapies that are involved in maintaining telomere length could improve the cardiovascular function of patients with heart failure. "With our test platform, we now want to clarify the question of who is the hen and who is the egg, whether the administration of telomerase could perhaps be effective in preventing heart failure and at what point we should specifically counteract telomere shortening in the heart muscle cells."
The original paper “Telomerase is essential for cardiac differentiation and sustained metabolism of human cardiomyocytes“ can be found here.
Text: Kirsten Pötzke