Replacing animal experiments: an MHH research team has succeeded in producing a haematopoietic heart organoid for the first time.
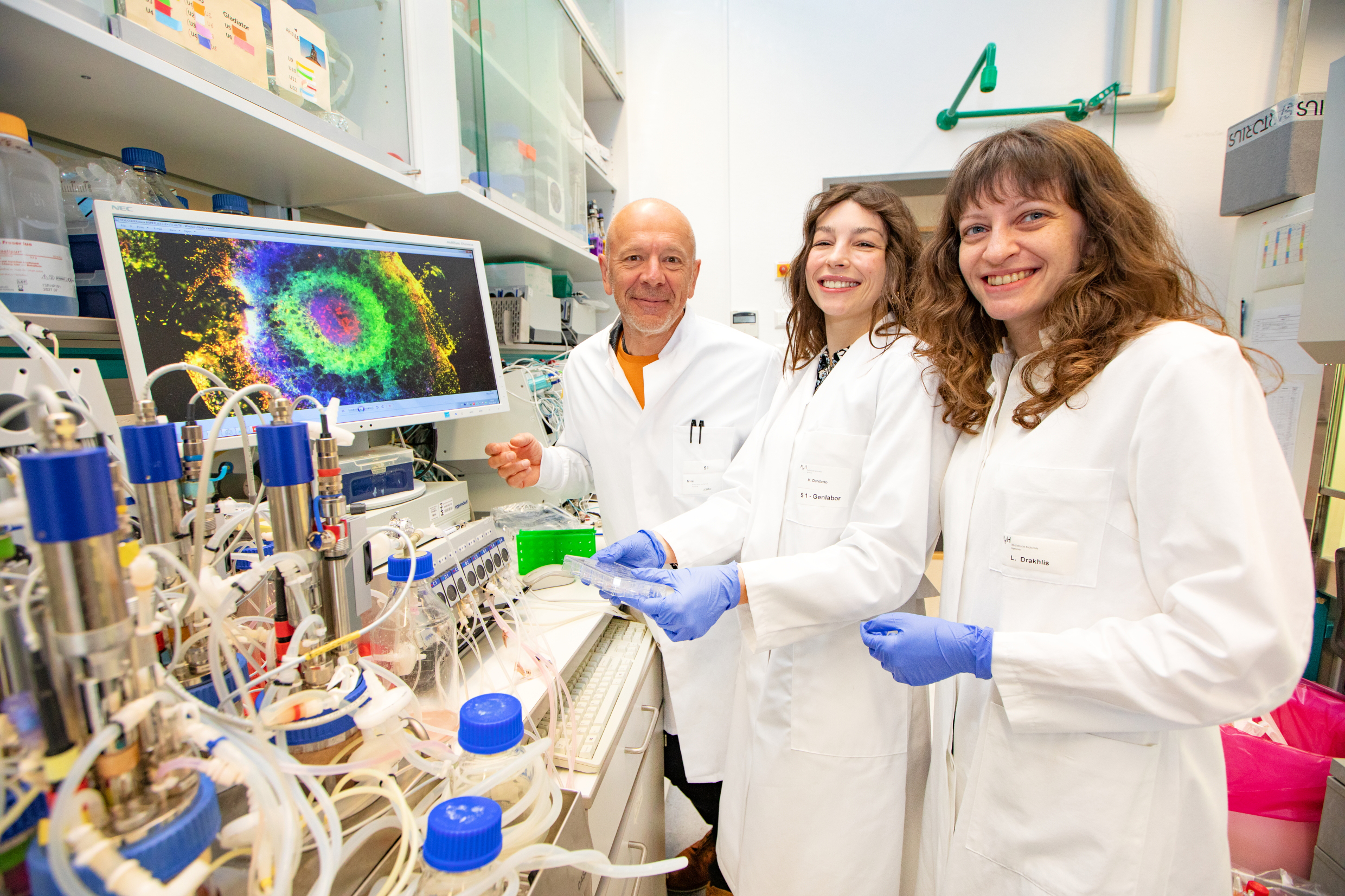
Dr Robert Zweigerdt, Dr Miriana Dardano and Dr Lika Drakhlis (from left) have developed a multi-layered haematopoietic mini-heart. Copyright: Karin Kaiser/MHH
How do human organs develop and what happens to them when they become diseased? To answer these questions, researchers are increasingly focussing on so-called organoids. These mini-organs, just a few millimetres in size, consist of groups of cells cultivated in the laboratory that can form organ-like structures. Similar to embryonic development, organoids make it possible to investigate the interaction of cells in three-dimensional space - for example in metabolic processes or disease mechanisms.
The production of organoids is tricky; the required nutrients, growth factors and signalling molecules must be added in a specific order and at specific times according to a precise schedule. In 2021, the research team led by Dr Robert Zweigerdt, cell biologist at the Leibniz Research Laboratories for Biotechnology and Artificial Organs (LEBAO) at Hannover Medical School (MHH), succeeded for the first time in producing a heart-forming organoid (HFO) and reproducing the entire path to the early stage of a human heart in cell culture.
One unsolved problem in science to date has been the development of a model that simulates heart development and haematopoiesis in combination. Haematopoiesis begins in the human embryo after the fourth week in the aorta, close in time and location to the cardiac anlage. Building on their heart organoid model, the researchers have now gradually added special factors and thus created a new, blood-generating heart organoid (blood-generating HFO, BG-HFO).This research success was recently published in the renowned journal ‘Nature Cell Biology’.
Tissue development like in an embryo
The mini-hearts are created from human pluripotent stem cells (hPSC). These are cells with special properties: they can be propagated indefinitely in culture and form any cell type. With the help of biological or chemical signals embedded in a hydrogel matrix, the hPSCs can be controlled in such a way that three-dimensional cell aggregates develop into cardiac organoids in ten to 14 days. These are not clusters of heart muscle cells, but complex structures consisting of at least seven different, clearly structured cell and tissue types.
As in natural embryonic development, the artificial mini-heart consists of three cup-shaped layers and comprises the anlagen of the heart, the precursors for the liver and lungs and the blood vessels.
‘We have now adapted our differentiation protocol, i.e. our special experimental instructions, and added a dense endothelial layer to the heart organoid, which lines the blood vessels and from which the blood-forming cells and progenitor cells emerge,’ explains Dr Miriana Dardano, first author of the scientific study. ‘This is the first human organ model of its kind that combines all tissues according to development in the embryo,’ says the stem cell biologist.
As flexible as a construction kit
‘Our study now enables other researchers to investigate in cell culture how the cross-tissue interaction in haematopoiesis takes place,’ emphasises Dr Lika Drakhlis, co-leader of the research work. However, the new findings are not only of interest to science for the elucidation of healthy organ development and haematopoiesis. The expanded haematopoietic heart organoid could also serve as a model for diseases such as COVID-19, which attacks the heart and blood vessels as well as the lungs. Infections with other viruses or bacteria, cancer or malformations caused by genetic defects could also be investigated in the cell culture dish to better understand and treat cardiovascular diseases. The organoids are also suitable for testing pharmacological agents. ‘In some cases, this works even better than in animal models, for example, because these are subject to other biological influences and the results can only be transferred to humans to a limited extent,’ says the scientist.
And because their principle of organoid production is as flexible as a construction kit, the LEBAO researchers are not stopping at the heart and blood. They are already working on a new differentiation protocol that converts the hPSC starting cells into cells from other organs so that further multi-tissue organoid models will be available for medical research in the future.
The original paper ‘Blood-generating heart-forming organoids recapitulate co-development of the human haematopoietic system and the embryonic heart’ can be found here.
Text: Kirsten Pötzke