Intensive Care Medicine
In order to answer clinical as well as scientific and translational questions as precisely as possible, we have established a cooperation of three large university associated intensive care departments in Germany and Switzerland, namely Bonn-Hannover-Zurich – the BonHanZA (Bonn-Hannover-Zurich-ARDS) study group. Co-PIs of this group are Prof. Sascha David (USZ, Zurich), Dr. Pedro Wendel-Garcia (USZ, Zurich) Prof. Christian Bode (UKB, Bonn), PD Benjamin Seeliger (MHH, Hannover) and PD Klaus Stahl (MHH, Hannover).
Our experimental interest lies on better understanding processes underlying the pathology of ARDS and septic shock, with a focus on the role of immune dysregulation and endothelial injury.
Clinically, we have initiated numerous retrospective and prospective collaborative studies that both evaluate existing therapeutic approaches in large patient collectives as well as investigate novel treatment options in patients with ARDS and septic shock. A special focus lies on evaluating current state of the art ECMO support as well as novel extracorporeal treatment modalities for septic shock.
From a translational aspect, we investigate the role of immune dysregulation and endothelial injury in predicting response to novel treatment options for ARDS and septic shock in a „bedside to bench“ approach.
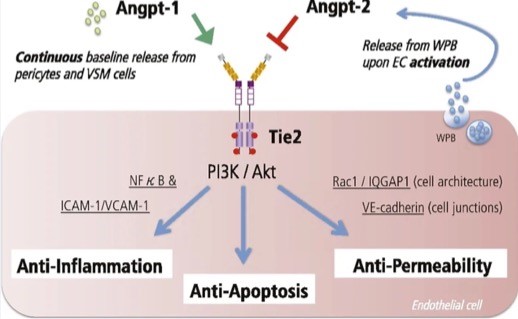
Our group is interested in molecular mechanisms regulating endothelial barrier function in response to inflammation. We have been focusing on the Angiopoietin (Angpt) / Tie2 ligand receptor system over the last decade. Tie2 is a transmembrane receptor tyrosine kinase that is essential for embryonic vessel development. In mature organisms, its function shifts toward maintenance of endothelial homeostasis and reaction to insults. Angpt-1 is the major circulating Tie2 agonist that promotes protective anti-permeability signals, whereas Angpt-2 has antagonistic properties. Our group was the first to prove in a murine knockout model that Angpt-2 directly contributes to sepsis morbidity and mortality.
Our group is interested in molecular mechanisms regulating endothelial barrier function in response to inflammation. We have been focusing on the Angiopoietin (Angpt) / Tie2 ligand receptor system over the last decade.
Tie2 is a transmembrane receptor tyrosine kinase that is essential for embryonic vessel development. In mature organisms, its function shifts toward maintenance of endothelial homeostasis and reaction to insults. Angpt-1 is the major circulating Tie2 agonist that promotes protective anti-permeability signals, whereas Angpt-2 has antagonistic properties. Our group was the first to prove in a murine knockout model that Angpt-2 directly contributes to sepsis morbidity and mortality.
Based on this finding we have conducted a series of experiments exploring potential therapeutic strategies (antibody, siRNA etc.) to eliminate or block the injurious Angpt-2 protein in sepsis models. We are also conducting drug-repurposing screens to identify potential off-target Angpt-2 regulators. Recently, we have gained much attention in the regulation of the Tie2 receptor expression per se and are currently working on the underlying mechanisms of posttranslational Tie2 modifications.
We are also interested in the interaction between endothelial cells and pericytes– both with regard to Angiopoietin signaling and the regulation of bioactive adrenomedullin (bioADM).
Another focus lies in the investigation of the endothelial glycocalyx both in vivo (SDF imaging) and in vitro (endothelial microperfusion chip model). As injury of the endothelial glycocalyx can be found early in critical illness and substantially contributes to endothelial dysfunction we investigate regulation of glycocalyx degradation both in septic shock as well as severe COVID-19.
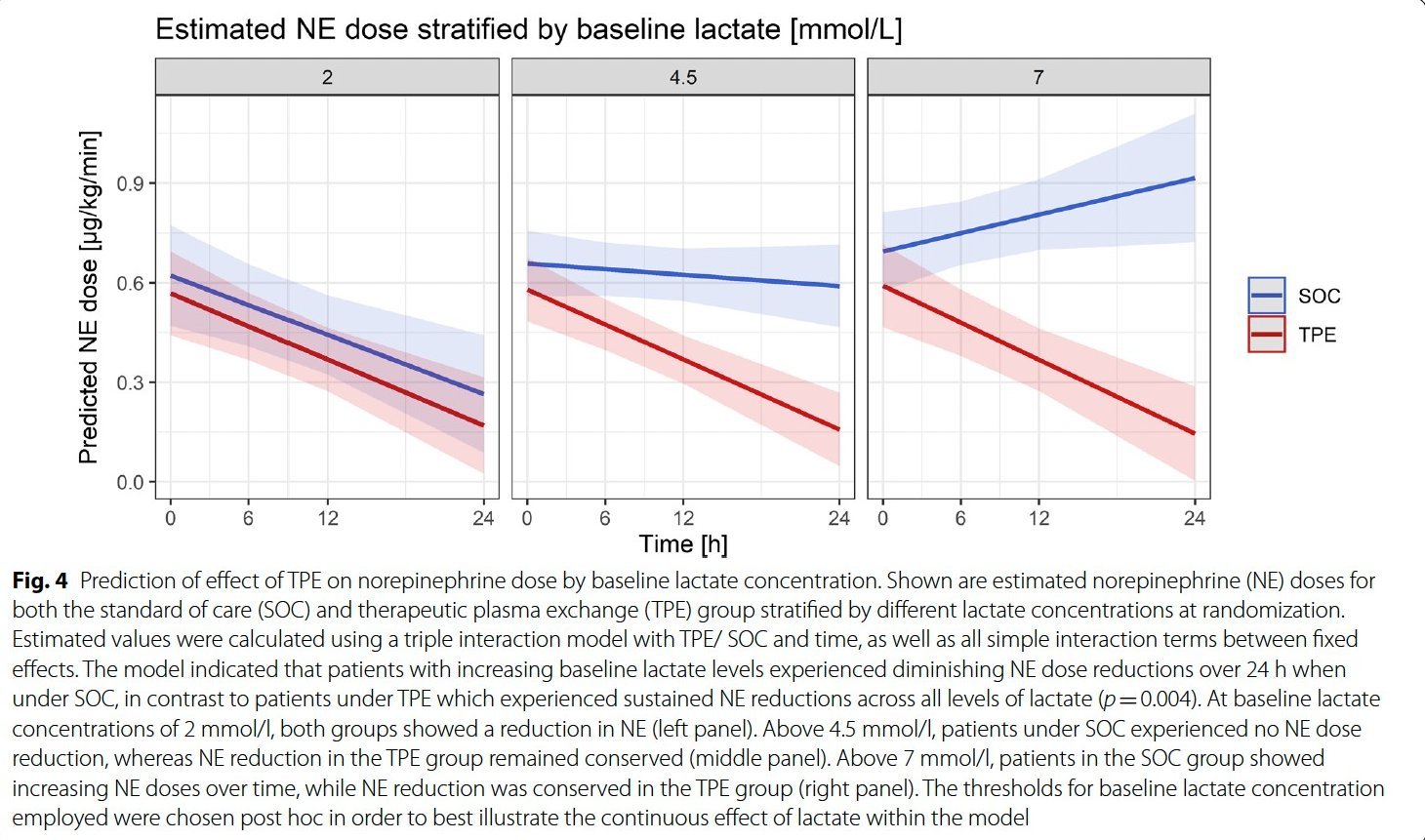
The hallmark of sepsis is a pathological host response to an infection that may lead to organ dysfunction, shock and ultimately to a high mortality. Besides numerous circulating mediators triggering an inflammatory cascade, vascular barrier breakdown and microvascular hypoperfusion, the consumption and subsequent lack of protective plasmatic factors additionally contributes to sepsis pathophysiology. A causative sepsis therapy that targets the pathological host response is still missing as selective inhibition of singular mediators such as TLR4 or TNF was so far not effective in humans.
We believe that therapeutic plasma exchange (TPE) might eliminate numerous circulating injurious mediators in a short intervention and simultaneously replace essential but already consumed protective factors. We have therefore initiated a study program investigating the effect of early TPE in patients with early refractory septic shock (EXCHANGE study program). In a prospective non-randomized pilot study, we could demonstrate that early TPE improves hemodynamics and endothelial permeability as well as reduces inflammatory cytokines in patients with septic shock (EXCHANGE Pilot). In a subsequent bicentric (Hannover and Bonn) randomized controlled trial, we could confirm this finding concerning the effect of TPE on rapid restoration of hemodynamic stability in a controlled setting (EXCHANGE I). Funding for a multicenter randomized controlled trial investigating use of TPE in septic shock (EXCHANGE II) was granted to our group by the DFG and the study is about to start recruiting in more than 20 centers in Germany, Austria and Switzerland.
Currently, we perform several translational investigations that further elucidate the molecular mechanisms of sepsis (e.g. endothelial dysfunction, glycocalyx injury, dysregulation of immune responses and coagulation) that are potentially all influenced by additive TPE as well as predictors of response to TPE.
Neutrophil extracellular traps (NETs) play a major role in pathophysiology of sepsis and ARDS as they are actively involved in hyperinflammation and microvascular coagulation. Together with our colleagues from Guy´s and St. Thomas NHS Foundation Trust, London, we have planned a multicenter randomized controlled trial to investigate the additive use of a NET specific adsorbing column in patients with sepsis and ARDS (NucCap study).

The biological heterogeneity that is encountered in sepsis and ARDS might contribute to the disappointing results of randomized controlled trials that studied the effects of pharmacological interventions in an unselected population. Precision medicine focuses on the identification of therapeutic strategies that are effective for a group of patients based on similar unifying characteristics. Since precision medicine approaches in non-critical care settings such as cancer treatment have been recently performed with success, we aim to understand the biological underpinings of sepsis and ARDS subphenotypes so that personalized therapeutic approaches can be applied.
To furhter stratify patients with sepsis and ARDS by both clinical and biological phenotyping, we have initiated a prospective register of patients with ARDS and sepsis (SPARE-14 register) in combination with a longitudinal human biobank (blood and bronchoalveolar lavage fluids). So far more than 250 highly characterized sepsis/ARDS patients have been included in this databank. We aspire to explore individualized patient characteristics, both concerning routine clinical parameters as well as non-routinely measured disease mediators, that might shape disease progression and response to treatment.
Although there is still a lack of clear data that support the use of Extracorporeal Membrane Oxygenation (ECMO) in severe ARDS regarding survival benefits, ECMO has emerged as a therapeutic cornerstone for many patients and its use is of major interest in modern critical care medicine.
Our group tries to better understand who might ultimately benefit from ECMO and is trying to improve the way ECMO support is performed (e.g. individualized choice of anticoagulation intensity). We also explore ECMO support in non-traditional patient cohorts such as patients with diffuse alveolar hemorrhage. Support of non-intubated patients with both chronic and acute lung failure with ECMO, termed Awake ECMO, is an innovative strategy as it potentially completely avoids the multiple potential side effects of invasive ventilation. We explore this strategy in highly selected patient cohorts with singular lung failure such as patients with Pneumocystis-associated ARDS.
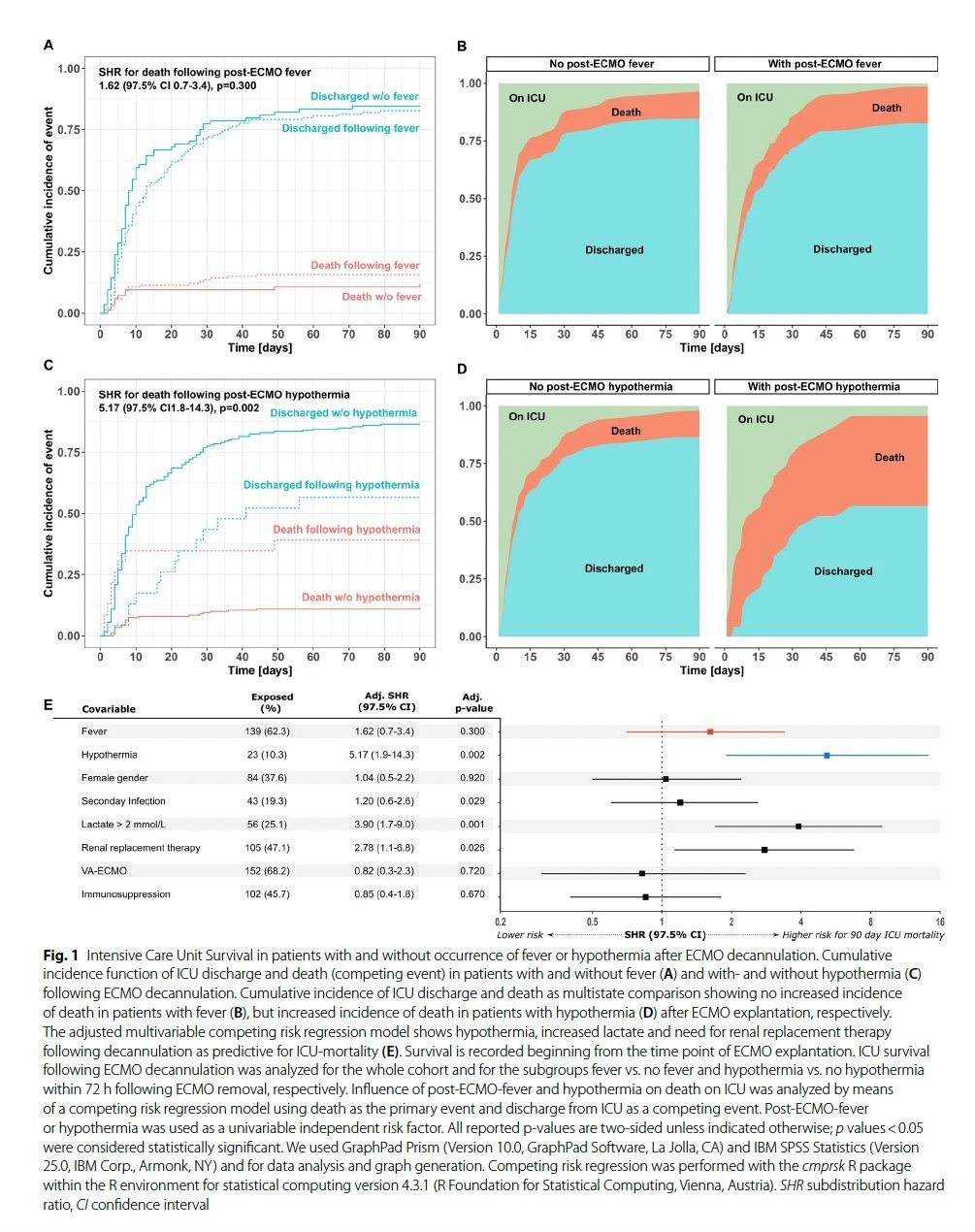
Fever after ECMO decannulation is a very common phenomenon which clinical significance however has been unclear to date. In a recent study we elucidated the role of hyper- and hypothermia following ECMO decannulation.

A work that analyzed the long-term outcome of triple cannulation ARDS patients who developed additional heart failure (VVA-ECMO) with Rolf Erlebach and Klaus Stahl in the lead was recently awarded with grants from the ESICM and the DGIIN.
Non-occlusive mesenteric ischemia (NOMI) is a life-threatening condition occurring in patients with shock and is characterized by vasoconstriction of the mesenteric arteries leading to intestinal ischemia and multiorgan failure. Although minimal invasive local intra-arterial infusion of vasodilators into the mesenteric circulation has been suggested as a therapeutic option in NOMI, current knowledge is based on retrospective case series and it remains unclear which patients might benefit. Our group has identified, togther with Jan Hinrich´s group, both early clinical indicators of NOMI and has prospectively analyzed predictors of response to intra-arterial therapy in patients with NOMI. We participate in a multi-center study to explore novel biomarkers for better diagnosing acute mesenteric ischemia (BIPAMI study).
Amatoxin related acute liver failure (AT-ALF) is associated with high mortality if no urgent liver transplantation (LTX) is performed. Therapeutic plasma exchange (PEX) has been demonstrated to improve LTX-free survival in patients with ALF of other etiologies. It is however unclear, if PEX may also improve LTX-free survival in AT-ALF and clinical practice in utilizing PEX in AT-ALF varies substantially between different centers. Of note, due to the scarcity of this ALF entity, realization of a randomized controlled trial investigating use of PEX in AT-ALF does not appear to be feasible in the future.
We (Richard Taubert, Bahar Nalbant and Klaus Stahl) initiated an ongoing multicenter, international, retrospective cohort study (Amanita-PEX study, NCT06187220) to investigate the effect of additive PEX compared to standard medical therapy (SMT) alone in AT-ALF. So far already 20 centers contributed more than 120 patients and a clear trend towards benefit of PEX in AT-ALF is observed. We are open for further centers to contribute.
Endoscopy
Our group is interested in various different open questions concerning state of the art interventional endoscopy with a special focus on biliary (ERC and PTBD) and EUS guided interventions as well as strategies to improve safety of endoscopic sedation (temperature control, CPAP ventilation).
Perioperative hypothermia is associated with significant complications and can be prevented with forced-air heating systems (FAHS). Whether hypothermia occurs during prolonged endoscopic sedation was however unclear and prevention measures were not addressed in endoscopic sedation guidelines. Our group (Henrike Lenzen and Klaus Stahl) hypothesized that hypothermia also occurs in a significant proportion of patients undergoing endoscopic interventions associated with longer sedation times such as ERCP and that FAHS may prevent it. We therefore performed a prospective observational study demonstrating that hypothermia in fact occurred in the majority of patients undergoing prolonged endoscopic sedation without active temperature control. FAHS was associated with higher temperature stability during sedation and better patient comfort. This study was honored by the first price of the DGE-BV in 2024.
Under the lead of Thomas von Hahn we will participate in a randomized controlled trial investigating whether the use of a simple nasal CPAP mask (SuperNO2VA™) compared to standard of care (i.e. nasal cannula with 2 l/min O2 flow) reduces hypoxemia episodes in obese and overweight patients undergoing upper endoscopy during propofol sedation administered by a non-anesthesiologist (non-anaesthesiologically administered propofol sedation (NAPS)).
Biliary strictures are among the most common complications following liver transplantation (LTX). If endoscopic retrograde cholangiography fails, percutaneous transhepatic biliary drainage (PTBD) may serve as an alternative approach. Description of clinical important short- and long-term outcomes as well as outcome prediction following PTBD after LTX are however scarce. Our group analyses both outcomes and outcome prediction in pediatric and adult patients receiving PTCD guided biliary therapy for biliary strictures following LTX.
The optimal time point of EUS-drainage of pancreatic ANCs still remains undefined. While the POINTER trial suggested to prefer later (> 4 weeks) drainage, it is unclear if very early drainage (< 2 weeks) is safe if needed to be performed in emergency situations. Together with Thomas von Hahn`s group from Hamburg we analyze in an ongoing project if very early (< 2 weeks) EUS-drainage of infected pancreatic ANCs is safe to perform in emergency situations and what are predictors of a favorable outcome.
Secondary sclerosing cholangitis (SSC) is a disease characterized by progressive destruction of the biliary tract and can be caused by a variety of stimuli, including toxic and infectious agents, immune-mediated mechanisms and ischemia. In recent years, a new subcategory of SSC in critically ill patients has been defined (SSC-CIP). SSC-CIP occurs weeks or months after the onset of a very broad spectrum of critical conditions, including severe trauma, burns, major thoracic or abdominal surgery, sepsis/septic shock and acute respiratory distress syndrome (ARDS). SSC-CIP often leads to recurrent acute cholangitis and cholangiosepsis, liver cirrhosis, hepatic decompensation and ultimately death. The prognosis of SSC-CIP is very unfavorable with an estimated 1-year survival rate of around 50%.
Treatment approaches for patients with SSC-CIP include endoscopic interventions using endoscopic retrograde cholangiography (ERC) with sphincterotomy, removal of gallstones, irrigation of the bile ducts, dilatation therapy, stent insertion or insertion of nasobiliary drains. However, it is still unclear which subgroups of patients with SSC-CIP benefit from such an intervention. At the same time, since ERC is an investigation potentially associated with severe post-procedural side effects, a more precise understanding of the predictors of expected therapeutic success under ERC in patients with SSC-CIP would be essential.
Histopathological characterization obtained by transjugular liver biopsy (TJLB) may theoretically contribute to clarification of the exact aetiology of acute liver failure (ALF). It's unclear whether the histopathological information from TJLB, due to the small specimen size, significantly contributes to diagnosing ALF causes, guiding therapy decisions, or predicting overall prognosis. In an ongoing study we analyze safety and clinical significance of TJLB in patients with ALF.
More information
Intensive Care Medicine:
- Prof. Dr. Sascha David, Institute of Intensive Care Medicine, University Hopsital Zurich, Switzerland
- PD Dr. Benjmain Seeliger and Prof. Dr. Marius Hoeper, Respiratory and Critical Care Medicine, Hannover Medical School
- Prof. Dr. Christian Bode, Operative Intensive Care Medicine, University Hospital Bonn
- PD Dr. Heiko Schenk and Prof. Dr. Hermann Haller, Nephrology, Hannover Medical School and Mount Desert Island Biological Laboratory, Maine, USA
- Prof. Dr. Michael Joannidis, University Hospital Innsbruck, Austria
- PD Dr. Christian Nusshag and Prof. Dr. Markus Weigand, University Hospital Heidelberg
- Prof. Dr. Samir Parikh, MD, BIDMC and Harvard Medical School, Boston, MA, USA
- Dr. Andrew Aswani, MD, PhD, Critical Care Medicine and Anesthesia, Guy’s and St. Thomas’ NHS Foundation Trust, London, UK
- Prof. Dr. Jan T Kielstein, Medical Clinic V, Nephrology, Rheumatology, Blood Purification, Academic Teaching Hospital Brunswick
- Prof. Dr. Jan Hinrichs, Interventional Radiology, Hannover Medical School
- Prof. Dr. Ulrich Budde, Hemostasiology, University Hospital Hamburg
- Prof. Dr. Malgorzata Wygrecka, PhD, Biochemistry, University Gießen
- The EXCHANGE-II study group (> 20 centers in Germany, Austria and Switzerland)
- The AMANITA-PEX study group (> 20 centers in Europe and North America)
Endoscopy:
- Prof. Dr. Thomas von Hahn, Academic Teaching Hospital Hamburg Barmbek
- PD Dr. Henrike Lenzen, Academic Teaching Hospital Brunswick
- Prof. Dr. Silke Leonhardt, Charite University Hospital Berlin
- Deutsche Forschungsgemeinschaft“ (DFG)
- Cytosorbents AG
- Santersus AG
Our Team
- Dr. Thorben Pape
- Dr. Bahar Nalbant
- Dr. Nina Rittgerodt
- Dr. Ann-Kathrin Rath
- Cand med. Eloise C. Schuette
- Cand med. Tabea von Garrel
- Cand med. Lea Plum
- The BonHanZA study group (https://www.bonhanza.com/)
- Dr. med. Philipp Gronski
- Dr. med. Philipp Wand
